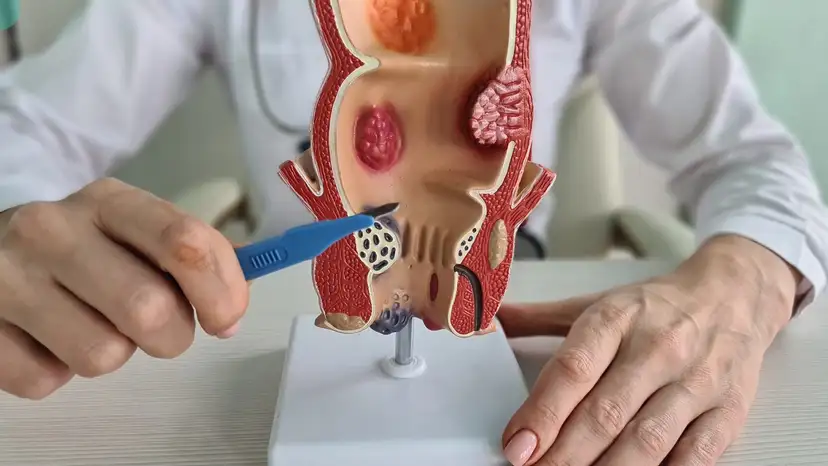
Understanding Anal Fistulas
An anal fistula is an abnormal connection that forms between the inner lining of the anus or rectum and the skin near the anus. It usually develops after an abscess, where a pocket of infection fails to fully heal. Patients may notice pain, swelling, redness, or discharge near the anal area, which can be persistent or intermittent. Simple fistulas affect only the superficial tissue, while complex fistulas involve deeper tissues and sometimes the sphincter muscles. Recognizing early symptoms is crucial because delayed attention can lead to chronic infections or more complicated surgical procedures. Some patients experience recurrent abscesses, bleeding, or difficulty controlling bowel movements. Early awareness of these warning signs can greatly improve the success of treatment and reduce the risk of long-term complications.
The Role of Early Diagnosis in Treatment
Early diagnosis is a key factor in successful anal fistula repair and removal guided by proper medical assessment. Diagnostic tools include physical examination by a colorectal specialist, MRI imaging, endoanal ultrasound, and fistulography. MRI scans provide detailed images of fistula tracts, helping doctors determine their complexity and involvement with sphincter muscles. Early detection allows surgeons to select less invasive techniques that preserve muscle function and reduce recovery time. Delayed diagnosis may increase the chance of recurrence or require more extensive surgery. Factors that may mask early symptoms include minor discharge, mild discomfort, or intermittent pain. Patients who address these signs promptly are more likely to experience smoother treatment and faster healing.
Treatment Options for Anal Fistula Repair and Removal
Anal fistula repair and removal guided by early diagnosis offers several surgical options depending on the type and location of the fistula. The main procedures include fistulotomy, fistulectomy, seton placement, and sphincter-sparing techniques such as advancement flaps. Fistulotomy involves opening the fistula tract and allowing it to heal from the inside out, often suitable for simple fistulas. Fistulectomy removes the entire tract, which can be effective for complex cases but may involve a longer recovery. Seton placement uses a surgical thread to keep the fistula open for gradual drainage, reducing the risk of abscess formation. Other advanced procedures aim to preserve sphincter function while closing the tract. Non-surgical management may include antibiotics or abscess drainage, but these are usually temporary solutions. The choice of treatment depends on the fistula’s complexity, patient health, and long-term goals of symptom control.
Preparing for Anal Fistula Surgery
Proper preparation is essential to maximize the success of anal fistula repair and removal guided by early diagnosis. Patients should undergo consultations and imaging studies to map the fistula accurately. Preoperative bowel preparation may be required to reduce infection risk and improve visibility during surgery. Lifestyle adjustments, such as avoiding certain medications or improving diet, can also support recovery. Anesthesia options and the expected duration of surgery should be discussed with the surgeon. Patients are encouraged to ask about postoperative care, potential risks, and expected outcomes. Mental preparation and understanding the recovery process can reduce anxiety and improve adherence to care instructions.
Post-Surgical Care and Recovery
Effective post-surgical care is critical for proper healing after anal fistula repair and removal guided by early diagnosis. Maintaining excellent hygiene and cleaning the surgical site as instructed by the doctor reduces the risk of infection. Pain management may involve prescribed medications or over-the-counter options, depending on the severity. Dietary adjustments, including high-fiber foods and adequate hydration, help prevent constipation and straining. Patients should monitor for warning signs such as fever, excessive bleeding, or foul-smelling discharge, which may indicate complications. Recovery timelines vary but typically include several weeks of restricted activity and gradual return to normal routines. Regular follow-up appointments allow doctors to track healing and address any issues early, minimizing the chance of recurrence.
Preventing Recurrence and Maintaining Long-Term Health
Preventing recurrence is an important aspect of anal fistula repair and removal guided by early diagnosis. Lifestyle choices such as maintaining a balanced diet, staying hydrated, and avoiding prolonged straining during bowel movements can reduce risks. Patients are encouraged to monitor their condition and report any changes immediately. Follow-up imaging may be recommended for complex fistulas to ensure complete healing. For individuals with underlying conditions, such as Crohn’s disease, proper disease management is crucial. Consistent communication with a colorectal specialist helps identify early signs of recurrence. Awareness of personal risk factors and adherence to postoperative guidance significantly improve long-term outcomes.
Patient Support and Resources
Support and education are vital for patients undergoing anal fistula repair and removal guided by early diagnosis. Access to support groups and online communities allows patients to share experiences and coping strategies. Reliable educational materials provide guidance on hygiene, diet, and recovery practices. Colorectal specialists can offer personalized advice based on the complexity of the fistula and the patient’s health status. Patients may also benefit from counseling or mental health support, as chronic anal fistula symptoms can affect emotional well-being. Family members and caregivers should be included in education to assist with care at home. Understanding the condition and recovery process empowers patients to actively participate in their healing journey.
Frequently Asked Questions (FAQ)
- What is the difference between fistulotomy and fistulectomy?
Fistulotomy opens the fistula tract to allow natural healing, while fistulectomy removes the entire tract. Fistulotomy is often used for simple fistulas, whereas fistulectomy suits complex or recurrent cases. - Can anal fistulas heal without surgery?
Most anal fistulas require surgical intervention for complete healing. Non-surgical measures may temporarily relieve symptoms but rarely resolve the condition permanently. - How long does recovery usually take after fistula surgery?
Recovery typically ranges from 4 to 8 weeks, depending on the procedure and fistula complexity. Some complex cases may require a longer period for full healing. - Is recurrence common after repair?
Recurrence can occur, particularly if the fistula was complex or inadequately treated. Early diagnosis and proper surgical technique significantly reduce recurrence risk. - Are there dietary restrictions during recovery?
High-fiber diets and adequate hydration are recommended to prevent constipation and straining. Avoiding processed foods and alcohol can also support healing. - How can complications be identified early?
Signs such as persistent pain, fever, swelling, excessive bleeding, or foul-smelling discharge should prompt immediate medical attention.
Takeaway
Anal fistula repair and removal guided by early diagnosis improves treatment success and reduces complications. Recognizing symptoms early, consulting a colorectal specialist, and following recommended surgical and postoperative care protocols are essential for optimal recovery. With proper preparation, adherence to care instructions, and support from healthcare providers, patients can achieve long-term relief and maintain overall colorectal health. Early intervention not only simplifies treatment but also significantly enhances quality of life for those affected by anal fistulas.